Most simply, a personalized medicine approach is about giving “The right person, the right management at the right time, in the right amount”. Personalized Medicine is patient-centred care that uses a patient’s data or molecular information to stratify disease, select a medication, provide a therapy, or initiate a preventative measure that is particularly suited to that patient at that particular time. The benefits of this approach are in its accuracy, efficacy, safety and speed, and the fact that a preventive approach can be implemented.
Currently, reactive medical care is the standard. For the most part, interventions are initiated after symptoms have appeared and damage is often irreversible. This greatly increases the management costs, disease burden, and results in poorer outcomes. Treatment often takes a trial and error approach – drugs are selected and then changed and adjusted until clinical efficacy is observed.

Preventive medical care is the goal. The PROOF Centre is developing strategies using predictive, diagnostic, or prognostic biomarker information to enable earlier and more precise diagnosis, and earlier interventions complemented by more individualized therapeutics. This not only involves pharmaceuticals but involves the ability to segment patients into various risk levels, and to identify the genetic, environmental and behavioural factors influencing disease progression. This personalized medicine approach is efficient, proactive and effective, and will improve patient outcomes and reduce overall treatment costs.
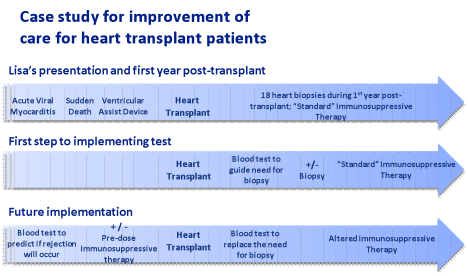
The following case study demonstrates how biomarkers will change medical care.
Lisa*, an 18-year-old, suffered irreversible heart damage from acute viral myocarditis and required a heart transplant. Before her transplant, Lisa underwent standard testing for viruses and immune markers and reactive antibodies. In her first year post-transplant, Lisa underwent 18 heart biopsies in addition to having “standard” immunosuppressive therapy, to ensure that her heart was not rejected.
As a first step to implementing our biomarker tests, we intend to implement a blood-based biomarker test which will indicate if a biopsy is necessary or not. Standard immunosuppressive therapy will still be required. This will be less painful and invasive for patients like Lisa, and we anticipate that we will be able to obtain more information from these tests than with a biopsy, and can gain more insight into Lisa’s condition.
In the future, our ultimate goal is to implement tests to predict if rejection will occur, and to allow immunosuppressive therapies to be administered early to prevent rejection. After transplant, blood tests will replace the need for biopsy, and as a result of pre-transplant personalized care, altered immunosuppressive therapy can be applied. Our hope is that by anticipating and preventing problems this early, that we will be able to profoundly change her post-transplant care, and ensure that her new heart is accepted and that she has the best health possible.
* this case study is based on an actual patient at the PROOF Centre, but her name has been changed.
